Medicaid Rollback is Still the Big Deal in the AHCA
Six weeks ago, when Congress first attempted to vote on the American Health Care Act (AHCA), it was primarily a bill that repealed Medicaid expansion.
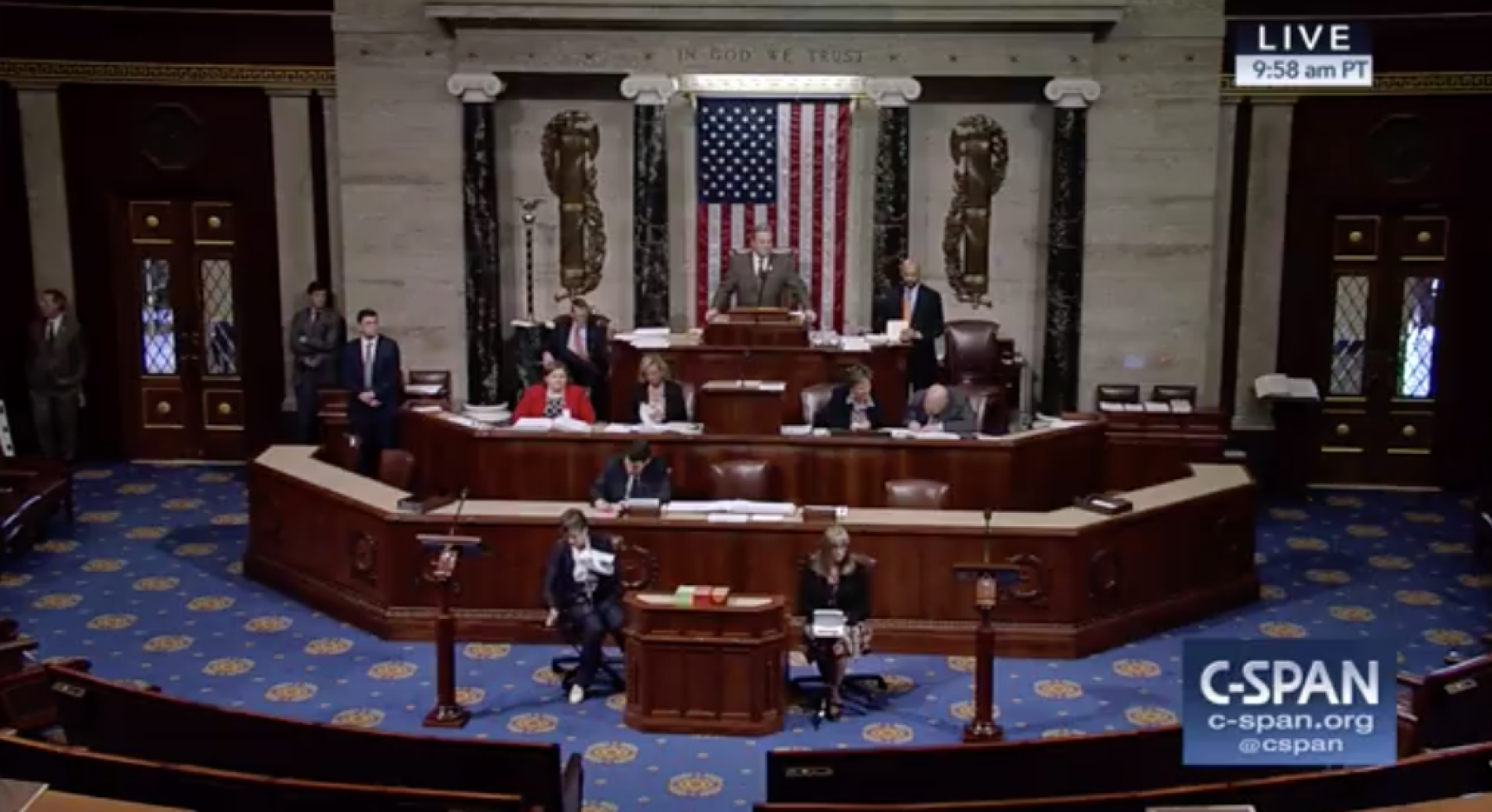
The House passed the bill today by the thinnest of margins, 217-213. But news coverage has lost sight of the biggest part of the AHCA: It is still a Medicaid repeal bill.
Nationwide, the federal government would save $880 billion over the next decade — money that would mostly be used to cut taxes imposed by the Affordable Care Act (ACA).
The Colorado Health Institute projected in March that the AHCA would all but eliminate the Medicaid expansion Colorado undertook through the ACA, leaving 600,000 Coloradans without coverage by 2030.
The amendments in today’s bill do nothing to change our projection.
One amendment allows states to maintain their Medicaid expansion for childless adults who make up to 133 percent of the federal poverty level; however, the federal government would pay half the cost, not 90 percent as it does under the ACA. CHI has already calculated that this reduction in federal payments would force Colorado to find nearly $1 billion a year to cover its Medicaid expansion — an impossible task in a state already struggling with budget constraints.
Our major conclusions about the AHCA remain largely unchanged:
- The bill whittles away at the ACA’s Medicaid expansion and converts Medicaid funding to per capita allotments.
- It bases tax credits for private insurance on age, rather than income and the price of insurance.
- It makes insurance cheaper for younger, healthier people and more expensive for older, sicker people.
- New today, states could allow skimpier insurance plans and higher prices for people with pre-existing conditions, as long as they have a program in place for high-risk insurance customers.
Today’s marquee amendments deal with the private insurance market. It’s too early to project the effects in Colorado. Most of the amendments were not released until 8:30 last night Washington time, and there is no new score from the Congressional Budget Office (CBO), which outlines the likely impacts on coverage and cost.
The updated AHCA adds funding for insurance companies to cover expensive patients. And it invites states to reduce minimum essential health benefits and allow insurance companies to charge more for people with pre-existing conditions, as long as states operate a high-risk pool. We doubt Colorado would do this under its current leadership.
A forthcoming report from CHI dives into the high-risk pool debate. (Pardon the awful pun.) It notes that the last federally financed high-risk pool in Colorado existed from 2010 to 2014 during the transition to the ACA. It covered 1,300 Coloradans at a cost of $90 million. That’s about $70,000 per enrollee over those five years. The amendment that appeared to secure the support needed for the AHCA to pass the House would add an extra $8 billion for high-risk pools. Based on Colorado’s experience, that money would cover just 115,000 people — nationwide.
At the same time, state legislators are considering a last-minute proposal, Senate Bill 300, to study high-risk pools and reinsurance. These are different methods of dealing with costly insurance customers. Whether either idea can work probably will depend on the fast-changing situation in Washington and the AHCA’s fate in the U.S. Senate.
By far, the AHCA will affect Medicaid enrollees the most. But CHI is keeping an eye on what will happen to other groups as well. Because of changes to how financial assistance is determined, those on the individual market who make less money or live in an area where insurance is especially expensive will find themselves paying more. So will older Coloradans. The law would also let states waive protections for age-based pricing or pre-existing conditions, and those waivers would likely hurt older and sicker residents.
This debate — which appeared to be over just a few days ago — still is far from finished.

