Sticker Shock: Prescription Drug Affordability in Colorado
The price of prescription drugs is rising, but the percentage of Coloradans who can’t afford them is falling. “Sticker Shock: More Coloradans Can Afford Prescriptions, but Problems Remain” analyzes data from the Colorado Health Access Survey.
While these findings may seem counterintuitive given headlines about rising drug costs, they make sense in light of the significant drop in Colorado’s uninsured rate from 14.3 percent in 2013 to 6.7 percent in 2015, a historic low driven by the Affordable Care Act (ACA). Essentially, because so many more people have insurance, they have better access to prescription benefits.
These important patterns emerge in the data: 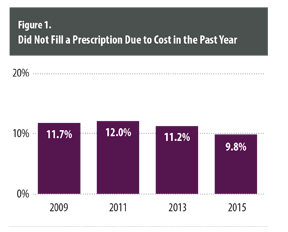
- Although Coloradans are gaining health insurance, that does not mean it is adequate health insurance. About 27 percent of the people who could not afford a prescription drug in 2015 were underinsured, meaning they have high out of pocket costs. That compares with 20 percent in 2013.
- The lowest-income Coloradans, those below 100 percent of the federal poverty level (FPL), are more than twice as likely as Colorado’s highest earners to not fill a prescription due to cost. However, they are having less difficulty affording prescriptions in 2015 than 2013.
- The closer Coloradans get to age 55, the more likely they are to forgo a prescription due to cost. About 15 percent of Coloradans between 45 and 54 did not fill a prescription due to cost.
- Only slight gaps were found among racial and ethnic groups. Nine percent of whites did not fill a prescription due to cost, compared to 12 percent of non-Hispanic blacks.
- The highest rates of those who didn’t fill a prescription because it cost too much are in the San Luis Valley (17.5 percent) and northwest Colorado (15.1 percent).
The affordability of prescription drugs is important because not filling a prescription can result in more hospitalizations and emergency room visits and increased illness.
This new analysis from the Colorado Health Institute addresses the following questions: Who is most likely to not fill a prescription due to cost? And has health reform affected Coloradans’ ability to afford prescription drugs?
Setting the Stage
Prescription drugs are playing a bigger role in the nation’s health care spending. They represented 9.3 percent of overall health spending in 2013, and are projected to grow to 10.4 percent by 2024. And while per capita prescription drug prices slowed between 2008 and 2013, they spiked in 2014, climbing an estimated 11.4 percent.1,2 Taken together, these data show why consumers and policymakers are concerned with prescription drugs.
How does Colorado’s spending on prescriptions compare to the rest of the nation?
The good news is that Coloradans had the lowest per capita spending on prescription drugs of any state in 2009, the latest year that data are available.3 While the data don’t indicate why this is happening, one theory could be that Coloradans tend to be healthier than the average american.
How many Coloradans can’t fill a prescription because it costs too much? And is that more or less than in the past?
About 500,000 Coloradans, or 9.8 percent of the population, did not fill a prescription due to cost in 2015, about 61,000 fewer people than in 2013. That’s the lowest percentage of people who said they couldn’t afford their drugs since 2009 (Figure 1). When the state’s economy was still experiencing the effects of the recession in 2011, the percentage was at 12 percent.
These numbers take into account all Coloradans, not just those who need a prescription.
How much do Coloradans spend on prescription drugs? And how does that compare to what Coloradans spent in past years?
Coloradans reported median out-of-pocket spending on prescriptions of $149 in 2015, about $45 less than in 2013, according to analysis of the CHAS. This decline in out-of-pocket costs could be due to the increasing number of Coloradans who gained health insurance through the ACA and no longer have to pay the full cost for medications.
There’s more to the story, however. The decline in the percentage of people who said they couldn’t afford their prescriptions wasn’t as large as we would expect. Colorado’s uninsured rate was cut in half, while the percentage of Coloradans who couldn’t afford a prescription only dropped by a few percentage points.
A Changing Health Insurance Landscape
A greater percentage of those who said they could not afford to fill their prescription were underinsured in 2015 than in 2013.
About 27 percent of the people who could not afford a prescription drug in 2015 were underinsured. That compares with 20 percent in 2013.
Here's what happened.
Increased insurance coverage also came with an increase in people who are underinsured, meaning they have coverage but their out-of-pocket costs eat up more than 10 percent of their annual income (five percent of income for those below 200 percent FPL).
These are usually people who enroll in plans with a low premium but high deductible, often known as bronze plans. As of December 2014, about 40 percent of Coloradans who enrolled in health insurance through the state’s marketplace, Connect for Health Colorado, bought a bronze plan.
Many people who were uninsured in 2013 transitioned into a health insurance plan by 2015 through private coverage or government programs like Medicaid or Medicare. Those programs cover prescription drugs, but to varying degrees.
But even people with adequate insurance sometimes have trouble affording drugs. More than a third (36 percent) of Coloradans who said they could not afford to fill a prescription were adequately insured.
Who is Most Likely to Not Fill a Prescription Due to Cost?
Insurance Type
Not surprisingly, Coloradans without health insurance were the most likely to report not filling a prescription due to cost in 2013 and 2015. This group generally needs to pay for medications entirely out of pocket.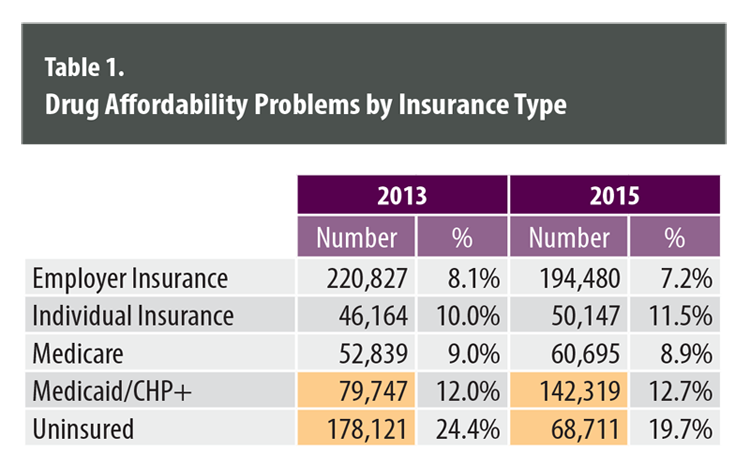
- The rate at which uninsured Coloradans reported not filling a prescription due to cost decreased to 19.7 percent in 2015 from 24.4 percent in2013, possibly as a reflection of the changing face of the uninsured (Table 1). Many sick and older Coloradans enrolled in Medicaid, so the uninsured pool was much smaller and made up of younger adults who may have not needed as many prescriptions.
- The Medicaid population expanded rapidly, and the percentage of Medicaid enrollees who could not afford a prescription rose slightly. It’s unclear why, but it may be because some people were enrolled in Medicaid only part of the year, or the drug was not covered by the program.
- Coloradans with employer-sponsored health insurance are the least likely to forgo a prescription due to cost, and they represent half of the Colorado population.
- Insurance status is one of the strongest predictors of not filling a prescription due to cost, according to a model created by the Colorado Health Institute. The odds were three to one that someone who could not afford a prescription was uninsured, rather than insured. People without insurance may have to pay completely out of pocket for expensive drugs, whereas insurance covers some of the cost for plan members.
Income
Coloradans on the lower end of the income scale were the most likely to not fill a prescription due to cost in 2015. However, even low-income Coloradans are having less difficulty affording prescriptions (Figure 2).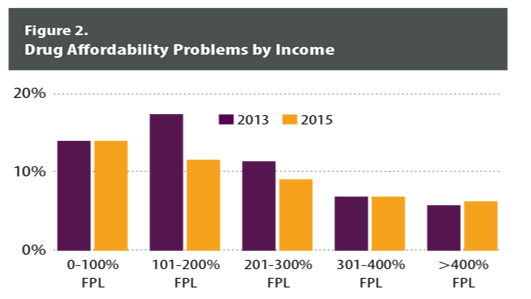
- The percentage of people between 101 and 200 percent FPL who couldn’t afford prescriptions declined significantly, to 11.6 percent in 2015 from 17.4 percent in 2013. This decline was most likely driven by expanded eligibility for Medicaid among this income group.
- Coloradans in the next lowest income bracket, 201 to 300 percent FPL, reported a two percentage point decrease in trouble affording prescriptions. ACA subsidies for private health insurance may have helped this group.
- The numbers did not decline for those between 301 and 400 percent of the FPL, even though financial assistance is available up to 400 percent FPL. It’s possible that these people were already able to afford health insurance without the help of the financial aid or that the subsidies were so low for this group they didn’t make a difference.
- It is unclear why there was no improvement in drug affordability for Coloradans below 100 percent FPL. Many in this group were able to enroll in Medicaid for the first time.
Age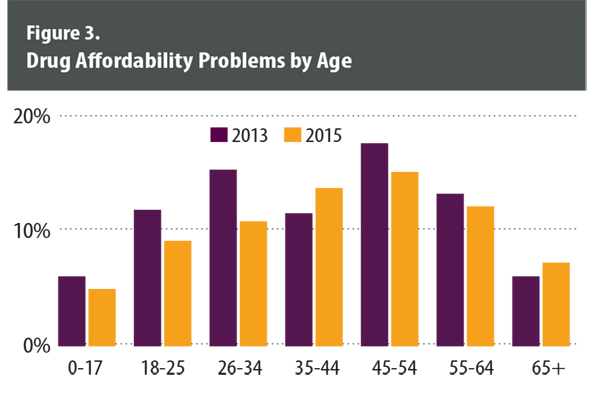
The closer Coloradans get to age 55, the less likely they are to be able to afford their prescriptions. However, almost every age category showed improvement from 2013 to 2015, most likely due to expansions in coverage (Figure 3).
- The percentage of Coloradans who didn’t fill a prescription due to cost tapers down after age 55 rather than after age 65, as might be expected when people qualify for Medicare. About 15 percent of 45- to 54-year-olds don’t fill a prescription because of cost compared to about 12 percent for 55- to 64-year-olds. One possible explanation: People in the 55- to 64-year-old category may purchase more comprehensive health care plans as they age and face greater health care needs.
- Those at the ends of the age spectrum were least likely to forgo a prescription. Children tend to be healthy, and seniors are almost all covered by Medicare.
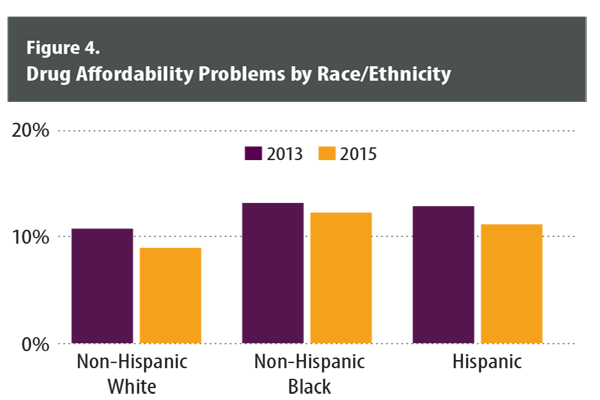
Race/Ethnicity
Racial and ethnic disparities in not being able to fill a prescription due to cost are minimal (Figure 4).
The percentage of non-Hispanic whites who could not afford a prescription due to cost dropped to 8.9 percent in 2015 from 10.7 percent in 2013.
Disparities by race are slight, with only a three- point difference between whites on the low end at 8.9 percent and blacks at 12.2 percent. Among Hispanics, 11.1 percent said they didn’t fill a prescription because it cost too much. One explanation may be that Hispanics do not use the health care system as often as whites, and therefore are less likely to have a provider write a prescription in the first place.
Health Status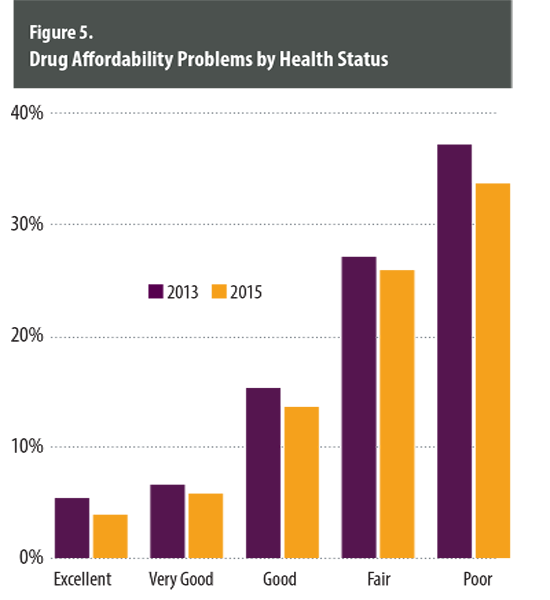
Coloradans in poor health are the least likely to be able to afford prescription drugs. Still, those in the poorest health appear to have benefited the most from the ACA (Figure 5).
- Drug affordability problems declined in every health status category. The percentage of those in the poorest health had the largest drop, to 33.7 percent in 2015 from 37.2 percent in 2013. Many of these people may have not been able to afford or obtain health insurance before the ACA because of a pre-existing condition.
- In 2015, poor health was, not surprisingly, the strongest predictor of not filling a prescription due to cost, according to a model created by the Colorado Health Institute. The odds were 5 to 1 that someone in poor health, rather than good health, would not be able to afford their prescription- when other factors such as income and insurance status are held constant. People in poor health have heightened health care needs and may need expensive specialty drugs.
Region
Pockets of rural Colorado have the highest percentage of residents who can’t afford a prescription (Map 1).
- The highest rates of those who didn’t fill a prescription because it cost too much are in the San Luis Valley (17.5 percent) and northwest Colorado (15.1 percent.) People living in these rural areas have lower incomes and are less likely to be able to afford prescriptions.
- Coloradans living along the Interstate 25 corridor, in the mountain regions and in southwestern Colorado tend to be the least likely to report forgoing a prescription due to cost. Those along the I-25 corridor tend to have higher average incomes.
- The residents of these communities also report better health status, making them less likely to need prescription medicines.
Policy Options
Despite the increase in health insurance coverage driven by the ACA, the price of prescription drugs continues to be a hot topic.
Decision-makers have taken note. State and federal legislative proposals around the country are aimed at understanding and lowering the cost of prescription drugs. President Obama’s 2017 budget contains proposals to increase the transparency of how pharmaceutical companies set drug prices and allow Medicare to negotiate prices.
State policymakers have introduced similar transparency measures, including one here in Colorado.8 The bill would have directed pharmaceutical manufacturers to submit reports about the most expensive drugs available in Colorado.9 Their reports would have been used to generate recommendations for controlling costs.
Pharmaceutical companies argue that drug pricing reflects the significant investment in research and development, and that they are being unfairly targeted to report proprietary information.
That argument seems to have traction, as most of the proposals have yet to become law. The proposed Colorado legislation failed when some criticized it for going too far and others said it didn’t go far enough.
Beyond pricing transparency, efforts by consumer advocacy organizations have called for more direct ways to help consumers, such as putting caps on total monthly copayments — rather just setting caps for individual drugs — to help those with chronic conditions who need several medications.10
It’s challenging to understand how often Coloradans forgo needed prescriptions. Some of them may never get a needed prescription in the first place because they do not have access to health care at a doctor’s office, clinic or hospital. Still, the ability to assess who is forgoing a prescription helps paint a richer picture of access to care.
This paper is part of the Survey Snapshot series. You can read the other Colorado Health Access Survey snapshots here