Colorado’s Unmet Demand for Specialty Care
Key Takeaways
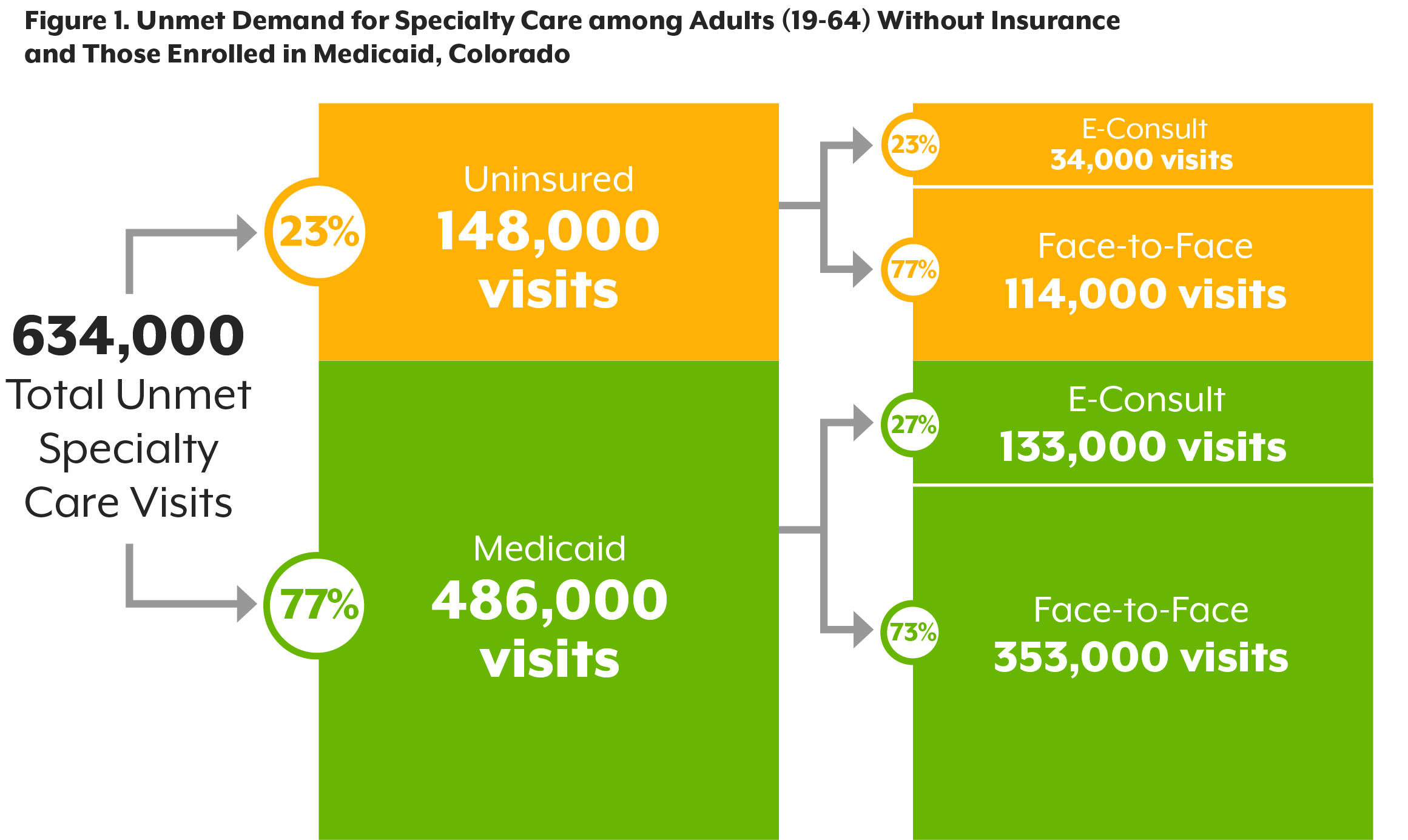
- In Colorado, Medicaid enrollees and people without insurance use specialty care at far lower rates than Coloradans with commercial insurance — illustrating a gap in access to care.
- Medicaid patients forgo an estimated 486,000 specialty care visits annually; for uninsured patients, it's 148,000 visits. On average, that’s about 87 extra visits annually for each of the state’s medical specialists.
- Addressing these gaps will require short-term and long-term solutions in the specialty care safety net — from increased use of e-consults and telehealth to initiatives such as increased use of advanced practice providers and more primary care provider education to address specialty care needs without a visit to a specialist.
Despite the best efforts of her primary care provider to get her an appointment, two offices turned down her insurance. She’s a member of Health First Colorado, the state’s Medicaid program, and the surgeons said they had reached their budgeted number of Medicaid patients for the year.
Now, Mya is on a waiting list to see an orthopedic surgeon at the local community hospital.
Mya is a real patient waiting for care in Boulder as of April 2019, and her experience is shared by hundreds of thousands of Coloradans annually who use Medicaid or have no coverage. These specialty care gaps persist despite Colorado’s decreasing uninsured rates and commitment to primary care access.
The Colorado Health Institute (CHI) estimates that 634,000 visits go unmet annually in Colorado because of gaps in insurance coverage, lack of specialist** capacity, and other barriers such as reluctance of some providers to accept patients who use Medicaid or who have no insurance. This report explains how CHI came up with that estimate and suggests several approaches to addressing the gap.
Colorado has employed many of the policy options available to states under the Affordable Care Act, from expanding Medicaid eligibility to building a state-based insurance exchange. Hundreds of thousands of Coloradans have benefited. Colorado has held on to its record-setting uninsured rate of 6.5 percent, according to the 2017 Colorado Health Access Survey (CHAS). (1) Colorado also has built strong primary care capacity — nearly 85 percent of Coloradans report that they have a usual source of care.
This is an abbreviated version of a more detailed report. You can download a PDF version of the full report here.
The story, however, is much different for specialty care, especially for low-income Coloradans. The median time that Coloradans wait for a general doctor appointment is two days, but it's more than nine days for specialist care. Some Coloradans report waiting up a year. And Medicaid enrollees report waiting 1.4 times longer than commercially insured patients to get specialty care. Medicaid enrollees are nearly three times more likely than commercially insured patients to report they didn’t get specialty care because they couldn’t find a provider who took their insurance. (2)
Many low-income Coloradans do not see a specialist at all because it costs too much. This includes about 13 percent of Medicaid and Child Health Plan Plus (CHP+) enrollees and nearly 30 percent of uninsured Coloradans. That’s compared to only 9 percent of commercially insured Coloradans.
The trend is the same when we compare the experiences of people of color versus their white counterparts. According to the CHAS, 13.6 percent of people of color skipped specialist care due to cost in 2017, compared with 10.3 percent of white, non-Hispanic/Latinx Coloradans.
We also know that specialty care access varies greatly by geography. Median wait times for specialty care range from 6.5 days in Douglas County to 13.2 days in some rural and frontier counties.
This work was made possible by the Telligen Community Initiative.
Special thanks to the members of Colorado’s Specialty Care Stewardship Council and the Access to Specialty Care Engagement Network (ASCENT) cohort. We also thank Kaiser Permanente Colorado for supporting those important initiatives.

Colorado’s Work So Far
Efforts are underway in Colorado to address these inequities.
For example, health care professionals are getting around long wait times, cost barriers, and workforce shortages using e-consults — digital communication between a general health care professional and a specialist to get specialty care advice without a face-to-face patient encounter. In other words, e-consults are generalist-to-specialist email systems.
E-consults are critical tools for addressing specialty care needs because they do not require a patient to schedule, get to, or pay for a face-to-face visit with a specialist. That’s why this analysis focuses on e-consults as a potential solution to address Colorado’s specialty care access gaps.
Other health care providers are using telehealth to connect patients with specialists over live video. Patients can use telehealth services to get care when a local specialist is unavailable. That said, they still require getting time with a specialist, and payment for the services.
Many primary care providers are also partnering formally and informally with specialists to offer patients in-person services when needed.
To connect these efforts at a high level of leadership, CHI convened the Specialty Care Stewardship Council (SCSC), a group of C-suite health care leaders developing a statewide specialty care safety net. Read more about the SCSC in the full report.
But these efforts have not closed the gaps, and each solution has limitations. For example, e-consults are not reimbursed by insurers. Telehealth services are, but broadband internet access is a barrier. And specialists earn more for treating commercially insured patients than Medicaid members or uninsured patients. In so doing, they avoid low Medicaid reimbursement and billing challenges and socioeconomic factors that make it harder for some patients to keep appointments and adhere to their care plan, such as lack of transportation and comorbidities such as substance use and mental illness.
With support from the Telligen Community Initiative, CHI set out to quantify the problem and find ways to solve it.

What We Found
- It would take 167,000 e-consults and 467,000 patient-provider visits to meet the unmet specialty care demand among Medicaid enrollees and uninsured Coloradans.
- Addressing the gap will require multiple specialty care safety net solutions, including e-consults, in-person visits, and telehealth capabilities.
- It would cost about $93 million annually — or $47 million if we account for Medicaid reimbursement — to cover all of Colorado’s unmet specialty care visits.
Imagining a Statewide Specialty Care System – And How to Finance It
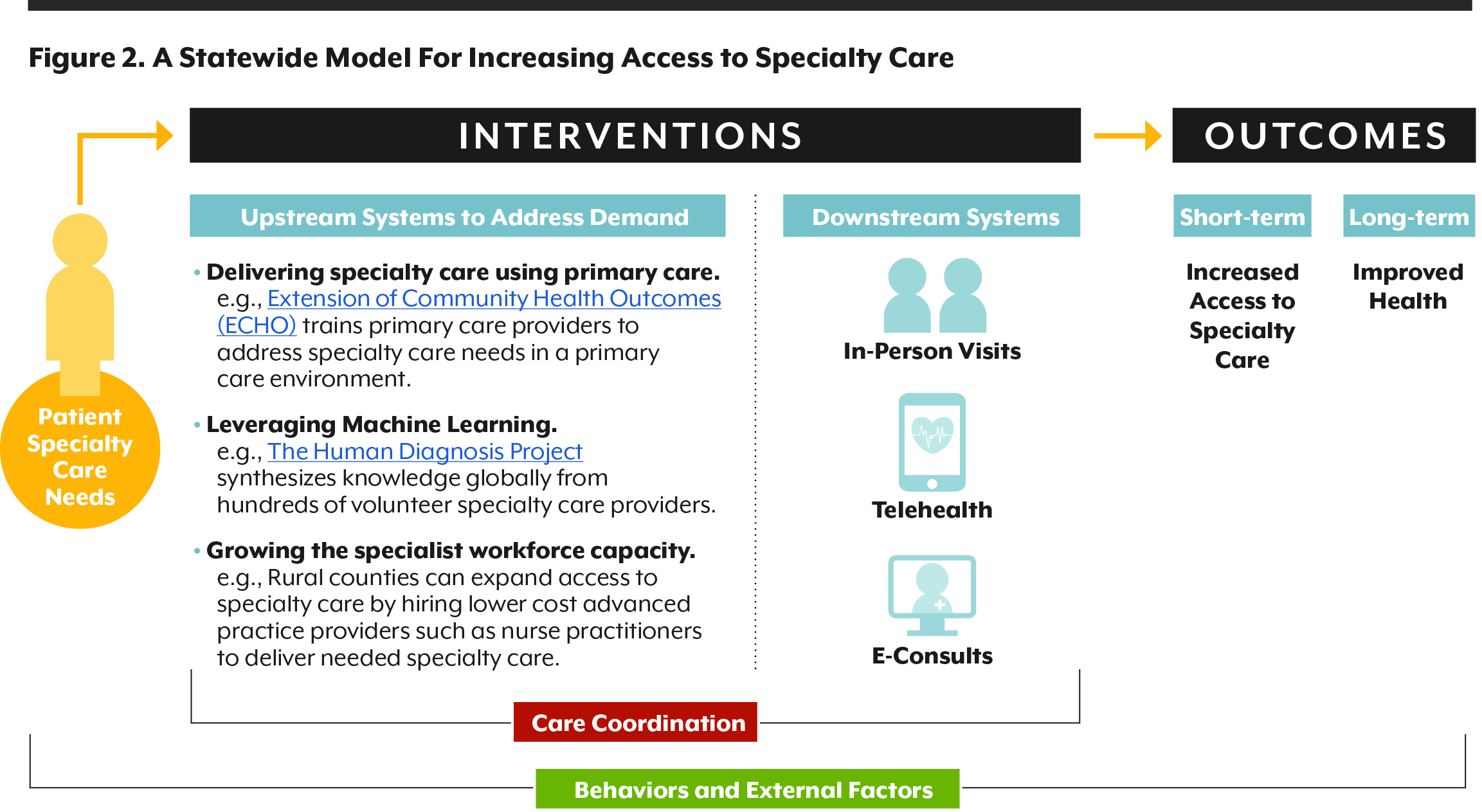
The statewide specialty care system that we envision will include e-consults, telehealth, and in-person visits. But the model will also invest in systems transformation to fundamentally change the way people access care, including:
- Provider education to promote specialty care access in primary care and non-traditional environments;
- Increased use of advanced practice providers such as nurse practitioners and physician assistants; and
- Emerging innovations such as machine learning that can increase access to specialty care.
This model is illustrated below. It was produced through partnerships between CHI and Colorado’s health care leaders.
Statewide Specialty Care Safety Net System Financing Options
- Short-Term:
- Create social impact bonds
- Funders provide capital and the state pays them back when program outcomes are achieved.
- Example in Colorado: Colorado's Coalition for the Homeless’ Social Impact Bond Initiative
- Policy Questions: Who could provide start-up funding? How do we measure the investment's success?
- Leverage health system community benefit
- Spending that promotes community health helps health systems retain their tax exemptions.
- Example in Colorado: Kaiser Permanente Colorado Safety Net Specialty Care Program
- Policy Questions: Do community benefit rules incentivize meaningful investments in critical issues such as specialty care access? How will these incentives change over time?
- Create social impact bonds
- Long-term:
- Change Medicaid reimbursement policy
- Colorado’s Medicaid program would reimburse for e-consults — or specialty care consultations delivered via electronic messaging.
- Example in Colorado: Colorado’s Medicaid 2016 rheumatology e-consult pilot program
- Policy Questions: How much would it cost to reimburse primary care providers for the time they spend on e-consults? How much would it cost to incentivize specialists to offer e-consults?
- Expand loan repayment initiatives
- Providers commit to practicing at a high-need site in return for loan repayment.
- Example in Colorado: Colorado Health Service Corps Loan Repayment Program
- Policy Questions: Will this option sustainably increase the number of specialists — especially those who serve uninsured and publicly insured Coloradans?
- Change Medicaid reimbursement policy

Policy Implications and Remaining Questions
CHI’s research reveals that addressing unmet specialty care demand will require multiple approaches. For example, any solution should include a mix of improved care coordination, education for primary care providers to address specialty care needs without a specialist, as well as face-to-face visits with specialists.
E-consults could provide a place to start. There is a mountain of evidence documenting their effectiveness increasing access to specialty care.(3,4,5) That said, expanding the use of e-consults raises multiple policy questions:
- What models exist for reimbursing e-consults? Should payment be limited to specialists or include primary care providers as well?
- Which types of visits, procedures, or services are more amenable to e-consults than others? Where could policymakers start?
- How long would it take for the state to realize a return on its investment in e-consults?
- What are the unique needs of rural areas? For example, to what extent are rural clinics equipped with broadband internet to support e-consults or telehealth? Is the specialty care provider workforce sufficient in rural areas to provide in-person referrals?
- What are the implications for licensure rules?
- What would it take for more providers to serve Medicaid members?
Conclusion
Analyzing Colorado’s unmet specialty care needs has illuminated the broad stakeholder interest in expanding access to specialty care for people who lack insurance or are enrolled in Medicaid. Challenging work is ahead — from selecting a model and implementing it, to making sustainable changes to the way Coloradans access specialty care via e-consult, telehealth, advanced practice provider, and other approaches. This analysis moves Colorado one step closer to expanding access to specialty care for everyone who needs it.
*Name changed to protect patient privacy.
**This report uses the term “specialist” to include any licensed provider of specialty care — including MD-trained providers as well as advanced practice professionals such as nurse practitioners, physician assistants, and others.
[1] Colorado Health Institute. (2017). “2017 Colorado Health Access Survey” https://www.coloradohealthinstitute.org/research/colorado-health-access-survey-2017.
[2] 2017 Colorado Health Access Survey
[3] Barnett, M.L., et al. (2017). “Los Angeles Safety-Net Program eConsult System Was Rapidly Adopted and Decreased Wait Times To See Specialists.” Health Affairs 36(3): 492-499.
[4] Olayiwola, J.N., et al. (2016). “Electronic Consultations to Improve the Primary Care-Specialty Care Interface for Cardiology in the Medically Underserved: A Cluster-Randomized Controlled Trial.” Annals of Family Medicine 13(2): 133-140.
[5] Fort, M.P., et al. (2016). “Implementation and Evaluation of the Safety Net Specialty Care Program in the Denver Metropolitan Area.” The Permanente Journal 21:16-022.