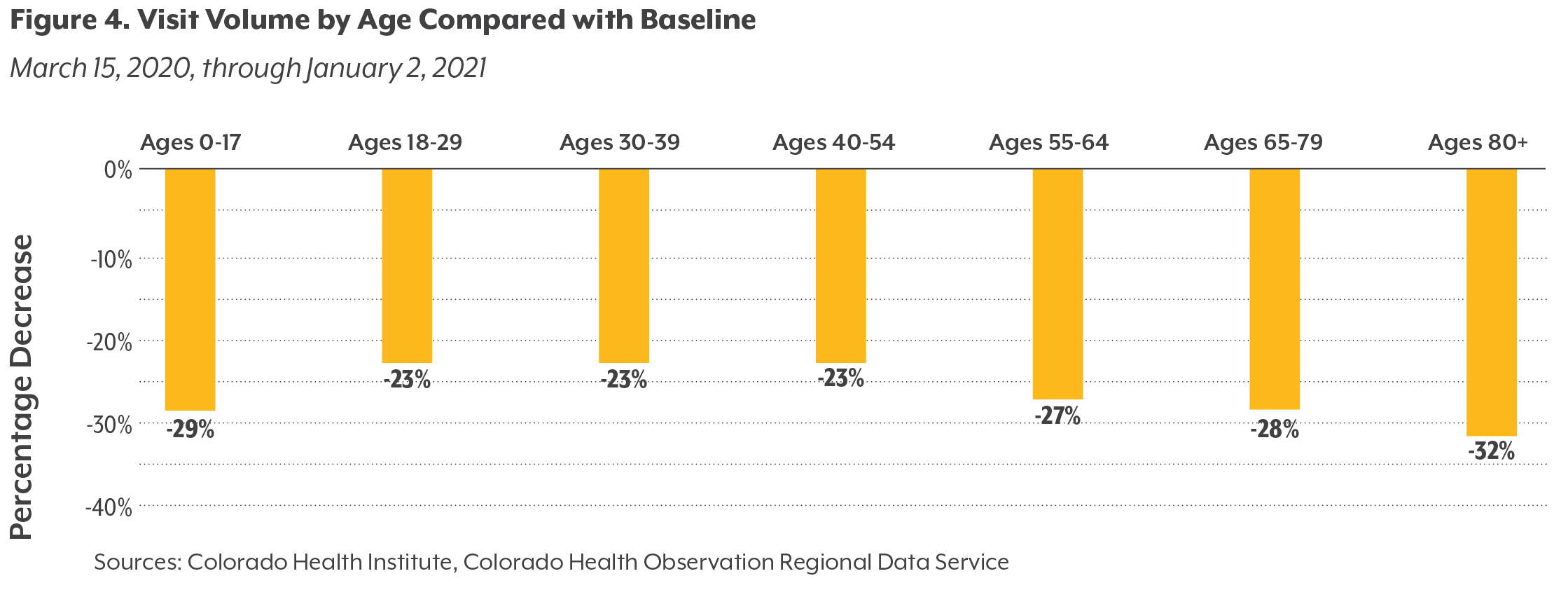
Missed Care Generally Increased with Age
The rate of missed appointments generally increased with patients’ age (see Figure 4), CHORDS data show. Care volume for Coloradans older than age 80 decreased by about a third (32%), while visits for those ages 18 to 54 declined by less than a quarter (23%). Older Coloradans may have been more likely to avoid in-person visits because of concern over the coronavirus; in addition, difficulties with technology may have discouraged some from using telemedicine as a replacement for in-person appointments. Because older Coloradans receive more health care on average than other age groups, they were also more likely to have an appointment cancelled or postponed during the early weeks of the pandemic.
Older adults are at risk for a decline in mobility and cognitive function due to reduced activity and isolation. In 2021, as the pandemic continues, physicians have reported their patients losing strength and having new difficulties with movement, balance, and weight control. Physicians also have seen an acceleration of conditions like dementia and worsening of illnesses such as diabetes, heart failure, and chronic obstructive pulmonary disease in elderly patients.
Children under age 18 missed more care than young adults ages 18 to 29. National data support this trend: Across the country, pediatric care saw steeper volume declines than other specialties. This is due in part to parents being forced to miss their children’s regularly scheduled well-child visits. Children under age 5 require many regular check-ups, particularly in their first year of life. From birth until age one, for example, Children’s Hospital Colorado recommends seven visits.
“We spent a lot of energy making sure we didn’t fall behind with the babies (those under age 2),” said a provider from Children’s Hospital. But healthy school-aged kids and teenagers, especially those not due for an immunization, had to be deprioritized and were more likely to miss preventive visits.
The provider points to two other key reasons why care volumes were down for children: less respiratory illness (including asthma) and fewer injuries, as kids were spending more time at home and less time socializing, in day care, or playing sports. Other health care providers, such as STRIDE Community Health Center, resumed well-child visits for those under age 2 as early as April 2020 and gradually expanded to serve older kids.
Visit volumes decreased slightly less for children under age 2 than for toddlers and preschoolers (ages 2 through 4) or elementary school-aged children (ages 5 through 12). This was likely due to an emphasis by pediatricians on well-child visits for their youngest patients in the early stages of the pandemic. Still, visits for this group were down by more than a quarter (29%) compared with the same period in 2019. Visits for teenagers (ages 13 through 17) decreased the least, by 27%, potentially because this population tends to have fewer regularly scheduled visits than younger children and because they can be more easily treated via telemedicine.
Early in the pandemic, some payers did not allow providers in Colorado to bill for virtual well-child visits. Some components of those visits, such as vaccinations, cannot be offered remotely, which may have also reduced care volume before in-person visits resumed. Once providers began offering in-person well-child visits again, not all families felt safe coming to a clinic and some may have believed that children who appeared healthy didn’t need an exam.
The Pandemic Exacerbated Existing Inequities
Among racial and ethnic groups, CHI’s analysis found populations with greater access to care prior to the pandemic were more likely to have missed visits during the pandemic. The sharpest declines in care were experienced by Asian Coloradans (32%), followed by white Coloradans (28%), Black Coloradans (25%), Hawaiian or Pacific Islanders (23%), and American Indian Coloradans (22%). Data from the Colorado Health Access Survey indicate that Asian and white Coloradans, like older adults, tend to use more care than Coloradans as a whole. Therefore, those with greater access to the types of care that can more easily be skipped and rescheduled later, such as preventive visits and health screenings, were more likely to miss care during the pandemic.
That is not the only factor at play, however. An analysis by the National Asian Pacific Center on Aging found that 42% of Asian Americans and Pacific Islanders are family caregivers, much higher than the rate in the overall population (22%). These multigenerational households and families may have taken additional precautions, such as avoiding unnecessary contacts and health care visits, to protect older family members. The rise in anti-Asian violence and hate crimes also may have deterred some Asian Coloradans from venturing out to seek care.
One national survey found that Black adults were more likely than white or Hispanic/Latinx adults to report delaying or forgoing care. A different national survey did not find significant differences in missed care by race or ethnicity.
This analysis is a step toward understanding the holistic impact of the pandemic on Coloradans’ health. However, it may underestimate the disparate impact on populations of color. The analysis compares changes in care volume with a baseline that suggests those populations have less access to — and less use of — health care due to historic, structural racism. Not surprisingly, someone who typically sees a medical provider several times a year was more likely to have had an appointment postponed, cancelled, or missed in the spring of 2020, when care volumes were at their lowest, compared with someone who sees a health care provider once a year, if at all.
Other data about the impact of the pandemic on communities of color are less equivocal: The various effects of the pandemic have fallen hardest on Black and Latinx Coloradans, who are more likely to get sick and die from COVID-19 and are being vaccinated at lower rates. A recent CHI analysis, also based on CHORDS data and focused on Front Range counties, found that infection rates were higher in Colorado neighborhoods where residents had lower education levels and in neighborhoods with more non-English speakers and people of color. Residents in these places may be more likely to hold jobs that require them to interact with the public and co-workers, increasing their chances for exposure to COVID-19 and making it difficult or impossible for them to practice social distancing. In the hardest-hit neighborhoods, CHI found that the rate of COVID-19 diagnoses was 10 times higher than in those neighborhoods that fared the best. It is possible that an increase in visits related to COVID-19 for populations of color may have played a small role in offsetting decreases in their use of other health care services during the analysis period, further complicating this analysis.
The pandemic also exacerbated inequities already present in Colorado, such as income inequality and disparities in access to food and stable housing. These changes will affect the long-term health outcomes of Coloradans and will not be felt equally among different racial and ethnic groups.
Emergency Department Use Decreased
A subset of emergency department use — visits by those who went to the emergency room and were sent home, rather than admitted for inpatient care — also decreased by around a quarter (25%), similar to the change in outpatient visits. Previous research by CHI found those patients who sought emergency care during the pandemic were sicker on average than emergency room patients prior to the pandemic, likely because they waited longer to seek care in an effort to avoid in-person interaction, particularly in the early months.
In many cases, patients delayed care for acute health issues such as heart attacks, strokes, and appendicitis — conditions for which prompt treatment is vital. A practitioner at STRIDE Community Health Center stated that their clinic frequently saw patients who put off care and were then forced to seek assistance in the emergency department. In an interview with The Longmont Leader, the director of UCHealth Longs Peak Hospital’s emergency department said patients who delayed seeking emergency care needed more aggressive treatment and faced a longer recovery. These outcomes could have been avoided if the individuals had gotten help when they needed it.
An Increase in Deaths
Other analyses have documented an increase in deaths in Colorado in 2020, many for reasons not due strictly to the pandemic. Excess deaths, a measurement of whether more people are dying than expected in a given year, were up across the board last year. Many of these deaths were directly caused by COVID-19, but others were due to secondary impacts of the pandemic, such as consequences stemming from missed health care.
While this analysis is not able to directly tie those excess deaths to the decline in care volume evident in the CHORDS data, the numbers are striking. According to a Denver Post analysis, there were almost 9,000 excess deaths in Colorado in 2020, of which almost 5,000 had coronavirus listed as either the underlying cause or a contributing factor. Deaths from Alzheimer’s disease, diabetes, chronic liver disease and cirrhosis, and Parkinson’s disease each increased more than 16% in 2020. Some of these deaths may have been prevented without so much missed care. Conversely, deaths from influenza and pneumonia were 23% lower than expected due to the success of social distancing and masking in lowering infection rates.
In a striking example of inequities exacerbated by the pandemic, age-adjusted death rates increased more than 30% for Latinx, Asian American, and Black communities in Colorado, while increasing only 8% for white Coloradans.
Making Up for Lost Time
The first step to ending the pandemic and improving Coloradans’ health is to continue the work of vaccinating people against COVID-19. Vaccination is the best tool available to tamp down the virus and allow our focus and resources to shift to supporting other aspects of the state’s recovery. But additional efforts to reconnect Coloradans with the health care system are urgently needed if we hope to prevent future epidemics of everything from cancer and chronic disease to behavioral health issues.
The focus of providers, policymakers, and local leaders should be on reaching out to patients and communities with tailored messages to mitigate health concerns that developed or worsened during the pandemic, and to head off negative health consequences that may develop further down the road.
Some recommended efforts and initiatives:
Providers should proactively reach out to patients with chronic illnesses, particularly those with comorbidities, to check on their health status and encourage them to seek care if they have not already done so. Insurers can assist by identifying and providing outreach and resources to their higher-risk members.
After many months spent isolated and stationary, a concerted effort is needed to identify and help some older Coloradans restore mobility and cognitive function.
Patients with new or worsening physical symptoms like occasional mild trouble breathing or behavioral health symptoms like anxiety should seek medical advice as soon as possible, even if these symptoms do not yet seem serious.
Many healthy Coloradans missed recommended wellness visits and screenings for cancer. The U.S. Preventive Services Task Force recommends annual screening for colorectal cancer in all adults starting at age 45, biennial breast cancer screenings for women starting at age 50, and annual lung cancer screenings for any adult older than 49 with a history of smoking at least 20 packs per year. Recommendations vary depending on medical history and should be discussed with a clinician.
To head off the spread of other (non-COVID-19) vaccine-preventable diseases, parents and providers should work to immunize children and youth who missed scheduled vaccines during the pandemic.
Behavioral health services, including substance use services, are more important than ever. Telemedicine has increased access to these services for many patients, but some will prefer and need in-person therapies.
Coloradans should speak with a provider if they have questions or concerns about their sexual health, as many routine visits and tests were skipped in 2020.
Dental care was not part of this analysis but is a key component of ensuring good health. Coloradans should schedule a dental appointment if they have not done so recently, and dental providers should connect with patients to encourage them to seek care — especially given that some undoubtedly experienced a year of increased stress-related teeth grinding.
Additional hurdles may complicate outreach efforts. For example, some Coloradans may need to find a new health care provider because their insurance plan’s network has changed since they last sought care or because their previous provider closed or retired during the pandemic. Continued access to telemedicine will help some patients, particularly those with behavioral health needs, maintain continuity of care. But many will face extra challenges with getting back into the doctor’s office. Health care providers and other leaders should think creatively about strategies and resources as they work to effectively assist those who need additional help.