Open Wide for Opportunity
The opportunity is the state’s launch of the Accountable Care Collaborative (ACC) Phase Two, the Regional Accountable Entities (RAEs), and the Alternative Payment Model (APM) in Health First Colorado, the state’s Medicaid program. These initiatives signal Health First Colorado’s commitment to reforming health care delivery through integrated care, new payment approaches, measurement, and connecting providers across disciplines in the “health neighborhood.”
This is a summary of the full report. The full report is available in a PDF here.
The RAEs and their partners — including the Colorado Department of Health Care Policy and Financing (HCPF), oral health professionals, members and their advocates, primary care providers, and the state’s third-party dental administrative services provider, DentaQuest — each play a role in improving access to evidence-based oral health care.
The potential benefits of expanding oral health care are far-reaching. Published evidence makes clear that the mouth is a window to the body. Improving oral health reduces the risk of serious physical conditions. And a healthy mouth absent of pain contributes to good mental health and is critical for social outcomes such as employment and the ability to learn in school.
In other words, oral health represents a prudent and beneficial investment.
Yet the need for oral health services in Colorado is significant, especially among people with lower incomes. One in four Coloradans (24.8 percent) with incomes at the poverty line or below report fair or poor oral health compared with just one in 10 (10.1 percent) Coloradans with incomes at or above 400 percent of the poverty line. About one third (29.7percent) of Coloradans report having no dental coverage. And fewer Coloradans with public insurance said they visited the dentist than those with private insurance — 60 percent compared with 74 percent.
The need may seem overwhelming. However, focusing evidence-based approaches for prevention and maintenance on key sub-populations of Health First Colorado members — such as children, people with diabetes, pregnant women, and older adults — represents a promising starting place. In doing so, Health First Colorado can lead a shift from the current volume-based payment and delivery paradigm that experts say contributes to these challenges.
The end goal is a more integrated system that addresses what the health care community commonly refers to as the Quadruple Aim: improved health, decreased cost, and improved experience for both patients and providers.
This Paper
The Colorado Health Institute, with support from the Caring for Colorado Foundation and Delta Dental of Colorado Foundation, developed this paper to examine the evidence behind oral health strategies, what other states have pursued, and what it would take for Colorado to implement its own approach.
This analysis aims to address one key question:
What opportunities exist for Health First Colorado and its providers to improve oral health by promoting evidence-based approaches?
In its research, CHI identified a core set of principles that guided this work. They include:
- Evaluate the evidence behind oral health strategies and commonly accepted practices.
- Focus on prevention and early intervention across the lifespan.
- Reconceptualize oral disease as a chronic disease.
- Reconceptualize oral health care as a component of primary health care.
- Assess a person’s risk for ongoing oral disease and deliver care based on individual risk.
- Deploy team-based care approaches, ensuring that oral health professionals — including dentists and dental hygienists — are working at the top of their licensure delivering evidence-based care.
As a starting point, CHI identified key populations with whom to prioritize efforts, including children, pregnant women, people with diabetes, and older adults. These are key segments of Medicaid enrollees for which there is evidence that suggests addressing — or preventing — oral health issues can avoid significant treatment costs and other diseases.
Applying the guiding principles resulted in CHI recommending four promising strategies aligned with the Quadruple Aim. They are summarized here but outlined in greater depth in the full report:
Strategy 1: Leverage Partnerships and Improve Provider Experience
Deploy oral health and primary care professionals to work in teams and ensure their skills are used efficiently and in ways that optimize what is permitted within their scopes of practice. This means developing meaningful partnerships among HCPF, medical and oral health providers, RAEs, member advocates and representatives, and Colorado’s Medicaid dental administrative services provider, DentaQuest.
Strategy 2: Reduce Health Care Costs
Incentivize prevention, risk-based care assessment, and innovative care delivery models by refining pay-for-performance metrics.
Strategy 3: Improve Health Outcomes
Ensure that Medicaid members have access to the right oral health care at the right place at the right time. This means expanding access to preventive services by integrating oral and physical health care, assessing a patient’s risk for oral disease, ensuring that care is coordinated among providers, and completing evidence-based treatment.
Strategy 4: Improve the Patient Experience
Maintain patient-centeredness throughout all the strategies. This includes promoting healthy behaviors and developing an oral health workforce that is informed about — and actively delivers — evidence-based, minimally invasive, and patient-centered care.
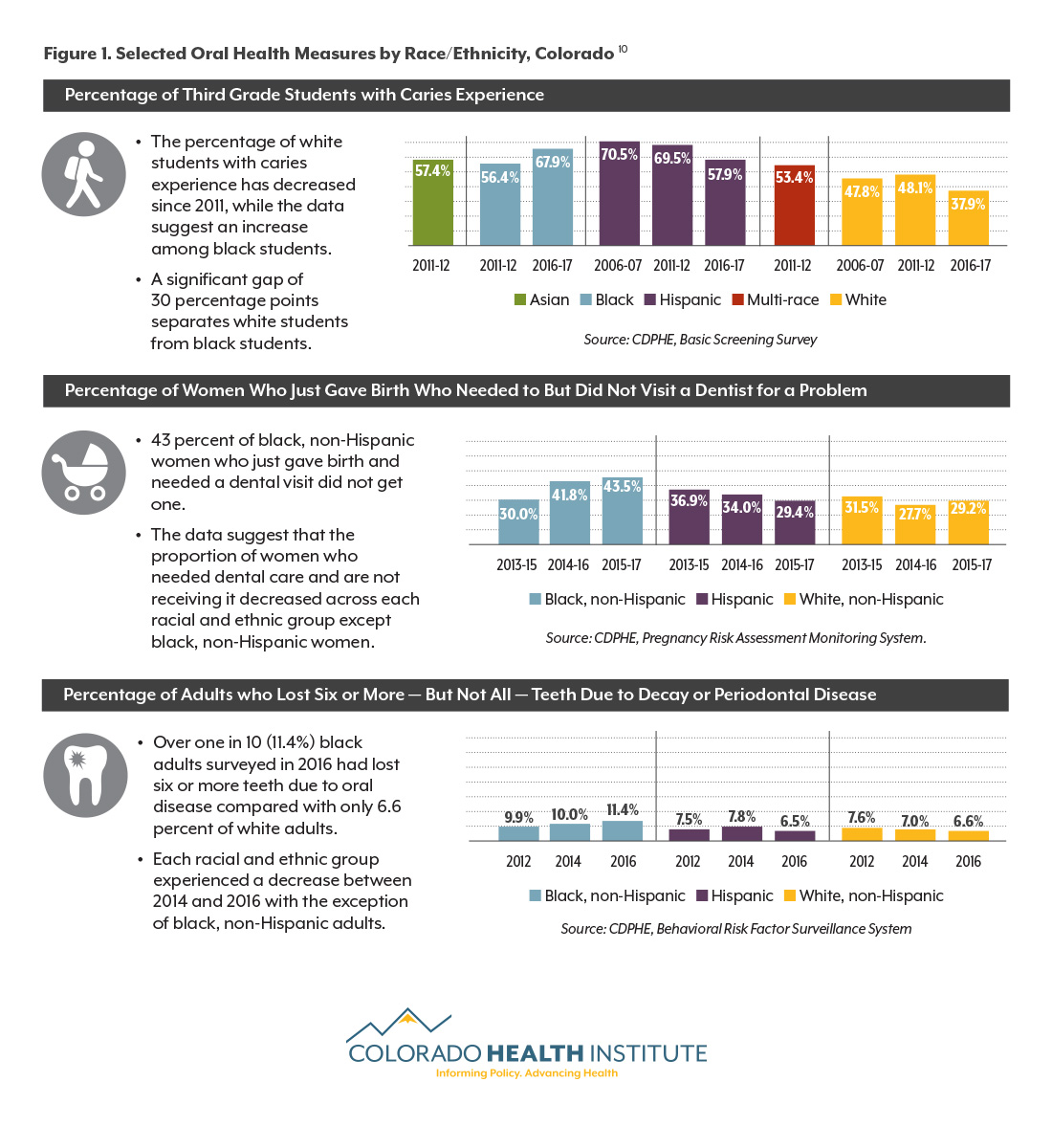
The demand for oral health care in Colorado is significant. Figure 1 explores oral health equity in Colorado. Many gains in oral health care over the past decade or two have not been equally distributed across people of different races and ethnicities. The graph illustrates the gap between non-Hispanic white Coloradans — often the most advantaged group — and Hispanic and black Coloradans, who disproportionately have lower household incomes.
CHI’s research shows that Health First Colorado can establish its leadership not only among public and private payers but also among other state Medicaid agencies in leveraging opportunities, evaluating them, and scaling them.